Could you be at risk of developing bowel/colon cancer? Despite efforts to raise awareness of the disease, it is still the second-leading cause of cancer death. Here’s what you need to know about colon cancer, and what you can do to prevent it from affecting your life or the lives of your loved ones.
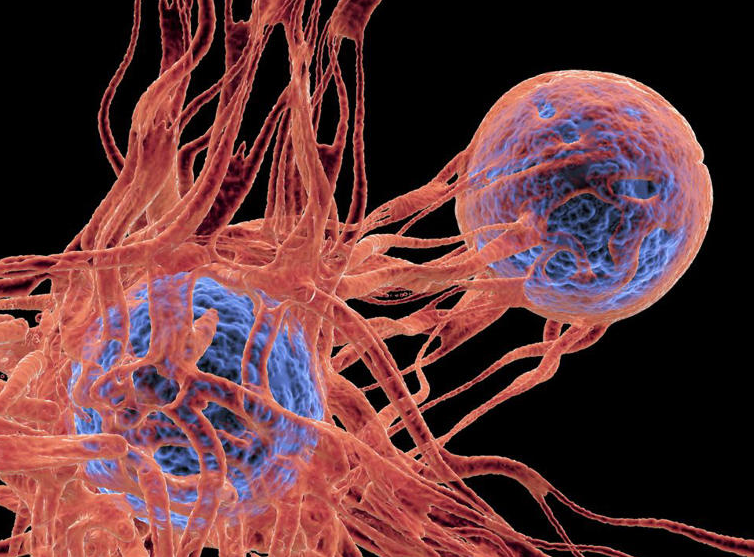
Colon cancer is a cancer that starts in the colon or large intestine. It shares many features with rectal cancer, and they are sometimes grouped together as colorectal cancer. It begins when cells in the colon start to grow abnormally, or out of control. Like other cancers, it can spread to other parts of the body if left untreated.
Most cases of colon cancer begin with polyps, which are abnormal growths on the lining of the colon. Although most polyps are benign, some can develop into cancer over several years. Adenomatous polyps, or adenomas, are considered pre-cancerous, and can be removed if detected early.
Family history, including some hereditary genetic syndromes, can increase an individual’s chances of developing colon cancer. According to the Mayo Clinic, people with hereditary nonpolyposis colorectal cancer (HNPCC), also known as Lynch syndrome, are very likely to develop colon or rectal cancer before they reach the age of 50.
People with inflammatory bowel disease (IBD) are more at risk of developing colon cancer and it is recommended that you start getting screened for colorectal cancer at a younger age and that you get screened more frequently.
Certain lifestyle choices can result in higher risk of developing colon cancer. Tobacco use, heavy alcohol consumption, and eating a lot of red or processed meat are all factors that can increase the risk of colon or rectal cancer. Individuals can also exercise regularly and avoid sedentary habits to reduce their risk.
Signs and symptoms of colon cancer include various bowel problems. If you are at risk for developing colon cancer and you notice any changes in your bowel habits, including chronic diarrhoea or constipation, rectal bleeding, or blood in your stool, you should see a specialist about possible causes. Other symptoms of colon cancer include unexplained weight loss and chronic fatigue.
More than half of people diagnosed with colon cancer don’t have any symptoms. The noticeability of the symptoms can vary depending on the cancer’s size and its location in the colon. This is why it is especially important for individuals to get screened regularly if they are at risk of developing colon cancer.
In its early stages, the most effective treatment of colon cancer is to remove the affected portions of the colon. When it’s caught early, surgeons might only have to remove a dangerous polyp, but more advanced cancer will require a partial colectomy, which is the removal of a portion of the large intestine.
In more advanced stages of colon cancer, chemotherapy may be necessary along with surgery. Not all doctors agree on when chemotherapy should be implemented, but the further the cancer spreads, the less likely it is that it can be removed solely by surgery. Chemotherapy is also used in cases where the tumour or cancerous area is too large to remove.
Together, colon and rectal cancer are considered one of the “major cancers” accounting for 11% of all new cancer cases. For males it is the third most common cancer with around 23,500 new cases in 2017, and the majority of those diagnosed were over 70 years in age.
In males in the UK, bowel cancer is the 3rd most common cause of cancer death with around 9,100 deaths in 2018. If colon cancer is detected early, the patient has a good chance of surviving. However, individuals diagnosed with stage IV, or metastatic, colorectal cancer have a low survival rate, highlighting the importance of early detection.
A person’s risk of developing cancer depends on many factors, including age, genetics, and exposure to risk factors (including some potentially avoidable lifestyle factors). 1 in 15 UK males will be diagnosed with bowel cancer in their lifetime.
54% of bowel cancer cases in the UK are preventable.
13% of bowel cancer cases in the UK are caused by eating processed meat.
11% of bowel cancer cases in the UK are caused by overweight and obesity.
6% of bowel cancer cases in the UK are caused by alcohol drinking.
7% of bowel cancer cases in the UK are caused by smoking.
2% of bowel cancer cases in the UK are caused by ionising radiation.
5% of bowel cancer cases in the UK are caused by too little physical activity.
28% of bowel cancer cases in the UK are caused by eating too little fibre.
A study published last year suggests that death rates for young people with colorectal cancer have been rising since the mid-2000s. Someone born in 1990 is twice as likely to develop colon cancer as someone born in 1950, and experts don’t know why.
The best way to avoid colon cancer is to get screened. In the UK men over a certain age get sent a test kit allowing them to screen themselves at home for colon or rectal cancer. This is mainly the stool DNA (sDNA) test, which both require the individual to send a stool sample to a lab to check for signs of colorectal cancer.
Statistics Source Cancer Research UK